Columbia University
Irving Medical Center
Neurological Institute
710 West 168th Street, 3rd floor
(212) 305-1818
Featured Research
In the Lab:
Yian Gu, MD, MS, PhD

Yian Gu, MD, MS, PhD
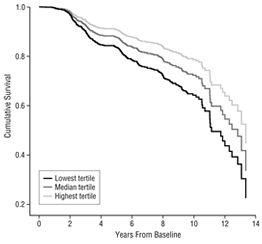
Figure 1
My research focuses on the nutritional epidemiology of brain aging, cognitive aging, Alzheimer's disease (AD), and other neurodegenerative diseases. My long-term goal is to elucidate the mechanisms for the diet-brain relationship by using multiple biological measures, including neuroimaging biomarkers, circulating biomarkers, genetic profiles, etc.
In collaboration with Drs. Richard Mayeux, Nicole Schupf, Jennifer Manly, Howard Andrews, and other Taub researchers, I work with data from the Washington Heights-Hamilton Heights-Inwood Community Aging Project (Dr. Richard Mayeux, PI) to understand the relationship between dietary factors and clinical cognitive and neurological outcomes in older adults. Dietary pattern analysis has a number of advantages, including the ability to capture complex interactions among dietary components and reduced concerns of measurement error and confounding by individual dietary components. In one study, I developed a dietary pattern to represent the dietary habits among the multiethnic WHICAP population. This dietary pattern was found to be associated with a 38% cut in the risk of Alzheimer’s disease (see Figure 1), a magnitude of protection similar to the Mediterranean-type diet (MeDi) that Dr. Nikolaos Scarmeas and colleagues found in the WHICAP population. Beyond Alzheimer’s disease, I have also collaborated with Drs. Karen Marder and Roy Alcalay to explore whether adherence to MeDi may delay the onset of Huntington's disease (HD) and Parkinson’s disease (PD).

Figure 2
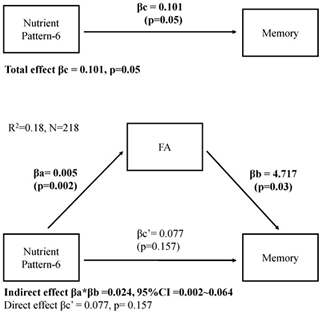
Figure 3
More recently, I collaborated with Taub Neuropsychologist Dr. Adam Brickman, PI of the WHICAP neuroimaging sub-study, to explore the association between dietary factors and structural neuroimaging markers of aging and neurodegenerative diseases. Our studies used imaging indices from multiple neuroimaging modalities, including brain volume, cortical thickness, white matter integrity, white matter hyperintensity, microbleeds, and other cerebrovascular diseases. We found that there was a strong positive association between the MeDi and brain volume (see Figure 2), and that moderate alcohol intake, one component of the MeDi, also showed some benefits on brain volume. In addition, we found that a healthy dietary pattern, characterized by high intake of omega-3 and -6 polyunsaturated fatty acids (PUFA) and vitamin E, was associated with both better white matter tract integrity and better cognition, and that white matter integrity mediated the relationship between this diet and cognition (see Figure 3).
In collaboration with Drs. Clinton Wright and Mitchell Elkind, I am in the process of performing replication analyses in the Northern Manhattan Study (Dr. Mitch Elkind, PI). Meanwhile, Dr. Yaakov Stern and I have found in preliminary analysis that more consumption of walnut, a food particularly rich in omega-3 PUFA, was associated with more favorable brain and cognitive outcomes among participants of the Reference Ability Neural Network Study and the Cognitive Reserve Study (Dr. Yaakov Stern, PI for both studies). These results are, to some extent, consistent with our previous findings that a 'PUFA-Vitamin E' dietary pattern was associated with better brain and cognition outcomes, and that higher dietary intake of omega-3 PUFA was associated with lower circulating level of β-amyloid.
Another goal of my research is to elucidate the underlying biological mechanisms for the beneficial effect of diet on brain and cognitive health. One such mechanism involves inflammation: we found higher circulating levels of inflammatory biomarkers (C-reactive protein and interleukin-6) are associated with less favorable brain MRI measures, such as smaller brain volume. Nevertheless, in collaboration with Drs. Nikolaos Scarmeas, Jose Luchsinger, and other WHICAP investigators, I found that C-reactive protein, a well-established inflammatory biomarker, did not seem to explain the association between MeDi and incident AD. While this study did not find a mediating role of single immune mediator C-reactive protein, in future, we will evaluate the inflammatory pathway by examining a more comprehensive panel of inflammatory and other relevant molecules.
Yian Gu, MD, MS, PhD
Assistant Professor (in the department of Neurology, Department of Epidemiology, and Taub Institute)
yg2121@cumc.columbia.edu

